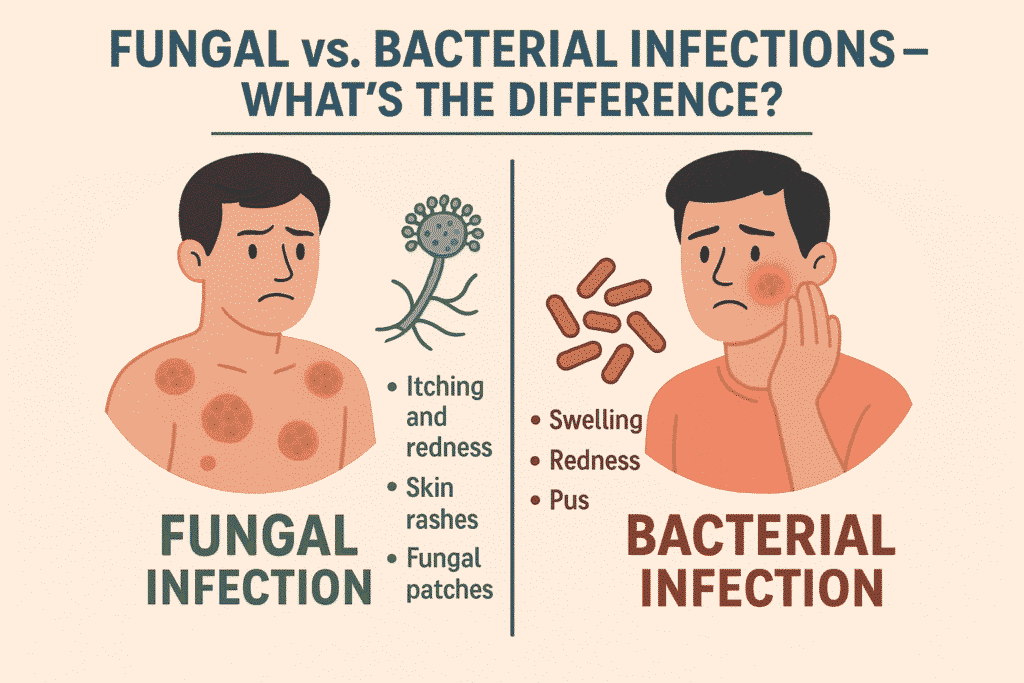
When we fall sick due to an infection, it’s easy to assume that all germs are the same. But did you know that fungal and bacterial infections are entirely different, from how they spread to how they’re treated?
Understanding the difference between Fungal vs. Bacterial Infections can help you choose the right treatment, avoid unnecessary antibiotics, and recover faster. Let’s break it down.
Main Differences Between Fungal vs. Bacterial Infections
Fungal vs. Bacterial Infections may look similar on the surface—causing symptoms like redness, swelling, or fever—but the organisms behind them are very different.
While bacteria are single-celled microorganisms, fungi are more complex, often multicellular, and thrive in warm, damp environments. Both can cause mild to severe diseases, but they differ in causes, symptoms, treatment, and even prevention.
Let’s compare both types based on several key factors:
1. What Causes Them?
| Factor | Bacterial Infections | Fungal Infections |
| Organism Type | Single-celled, prokaryotic organisms | Eukaryotic organisms (can be unicellular or multicellular) |
| Common Examples | Staphylococcus, E. coli, Streptococcus | Candida, Aspergillus, Trichophyton |
2. Where Do They Occur?
- Bacterial infections commonly target areas like the throat, respiratory system, skin, and urinary tract
Fungal infections commonly occur on the skin, nails, mouth, genitals, or lungs (in immune-compromised people).

3. How Do They Spread?
- Bacterial infections can spread via:
- Direct contact
- Contaminated food or water
- Airborne droplets (cough/sneeze)
- Fungal infections spread through:
- Skin-to-skin contact
- Shared clothing or surfaces
- Overgrowth of fungi already present on the body
4. Symptoms Between Fungal vs. Bacterial Infections
| Bacterial Infections | Fungal Infections |
| High fever, pus formation, swelling | Itching, redness, flaking skin, discharge |
| Rapid onset, pain, localized inflammation | Slow-growing, chronic or recurrent symptoms |
| Fatigue, body aches, sore throat | Slow-growing, chronic, or recurrent symptoms |
5. Diagnosis
- Bacterial infections are diagnosed via:
- Blood tests
- Urine or sputum cultures
- Throat swabs
- Fungal infections are diagnosed through:
- Skin scrapings
- KOH test (potassium hydroxide)
Fungal cultures or biopsies
6. Treatment of Fungal vs. Bacterial Infections
| Bacterial Infections | Fungal Infections |
| Treated with antibiotics | Treated with antifungal medications |
| Overuse can lead to resistance | Often topical, sometimes oral or IV |
| Faster response to medication | Treatment duration may be longer |
Important: Antibiotics do NOT work on fungal infections. Misusing antibiotics can worsen your condition.

7. Prevention Tips
- Maintain good hygiene.
- Avoid sharing personal items like towels or razors.
- Wear breathable fabrics to prevent moisture buildup.
- Always complete prescribed treatments—don’t stop halfway.
Boost immunity with a healthy lifestyle.
Fungal vs. Bacterial Infections (FAQs)
Q1. Can a fungal infection turn into a bacterial infection?
Q2. How do I know if my infection is bacterial or fungal?
Q3. Are fungal infections contagious?
Q4. Can I treat both infections with the same medicine?
Conclusion
Knowing whether your infection is fungal or bacterial is crucial for the right treatment. While they may appear similar, they behave very differently and need specific medications. If you’re unsure about your symptoms, consult a healthcare professional for proper diagnosis and avoid self-treatment with antibiotics or creams.
Your skin and body deserve the right care—identify the infection early, treat it correctly, and prevent it smartly!